I have this problem that I don't know how to deal with. and hope you can give me some pointers/suggestions.
I am with Aetna HDHP and I asked for routine eye exam as usual---no that I had or have any problem with my eyes, but Aetna policy says routine eye exam is 100% covered and I also received letter from dr's office reminding for annual routine exam.
I called for the routine exam and when I entered the office I also told them I was in for routine exam. As usual it's mostly Dr.'s assistant did all those exams, she only asked who my primary physician is and spent most of time entering data on computer. then Dr. came in for final check and asked about my diabetes ( I am on broadline diabete for more than 10 years) and any problem with eyes? I said no except the usual eye blurring (have been for 5 more years). then dr. said you're fine, no problem.
Then came the shock---Aetan pays nothing on this exam and I expect to pay out of pocket of $330 (deductible). Aetna said what my dr office submission was coded for medical diagnosis. I called dr's office and his manager said she didn't see routine box checked so it must not be routine and that I have diabetic problem. She said don't expect dr to change the coding and that she didn't want to talk about it any more and hung up the phone.
My husband, who doesn't have any medical problem, also went for routine eye exam at the same dr. office but by different dr.(I think he's the partner of my dr.), also end up pay $95--even he emphasized twice he want for routine check.
So the problem is not Aetna. It's not in the best interest of Aetna to help me to deal with Dr. because it would be glad not to pay anything expecting deductible from us. We've been with the same eye Dr. for many years for annual routine exams and Aetna paid most parts and we paid some small amounts <$50 for this and that extra exam Aetna said not within its policy. I was lazy to fight for those small amounts and ate them all.
But this time is really blowing out of water with $400+ out of pocket.
What should I do? any suggestion where to start to take actions?
Thanks in advance.
From: sarah_oz@yahoo.com [TSP_Strategy] <TSP_Strategy@yahoogroups.com>
To: TSP_Strategy <TSP_Strategy@yahoogroups.com>
Sent: Fri, Feb 19, 2016 7:21 am
Subject: [TSP_Strategy] Health Plan Changes
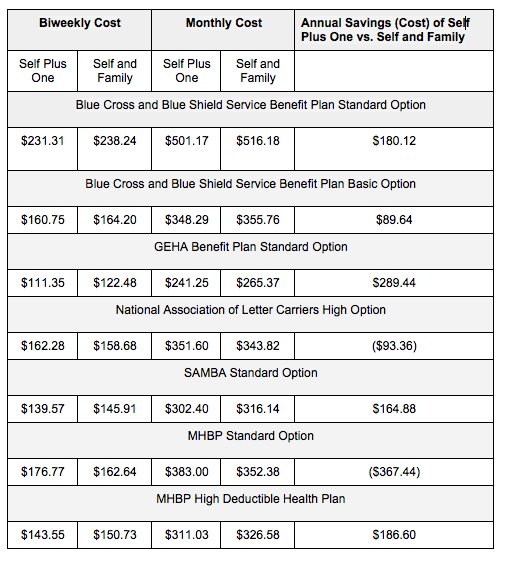
Another Chance for Health Plan Changes
Posted by: lindalyc@aol.com
| Reply via web post | • | Reply to sender | • | Reply to group | • | Start a New Topic | • | Messages in this topic (2) |

Belum ada komentar untuk "Re: [TSP_Strategy] Health Plan Changes"
Post a Comment